 The temporomandibular joint (TMJ) is essential for speech and eating. When it’s damaged or diseased, enjoying food and speaking with confidence becomes limited. Changes in the facial aesthetics can also increase self-consciousness. As such, quality of life is affected.
The temporomandibular joint (TMJ) is essential for speech and eating. When it’s damaged or diseased, enjoying food and speaking with confidence becomes limited. Changes in the facial aesthetics can also increase self-consciousness. As such, quality of life is affected.
Condylar joints are found across the body and support flexible movements.i For the jaw, the two condyles support talking, eating and breathing. Damage to the condyles therefore damages the TMJ.ii Condylar resorption is a disease associated with temporomandibular disorder (TMD), and dental practitioners should be encouraged to identify its risk factors and know how to treat it. This will help at-risk patients live a happier life.iii
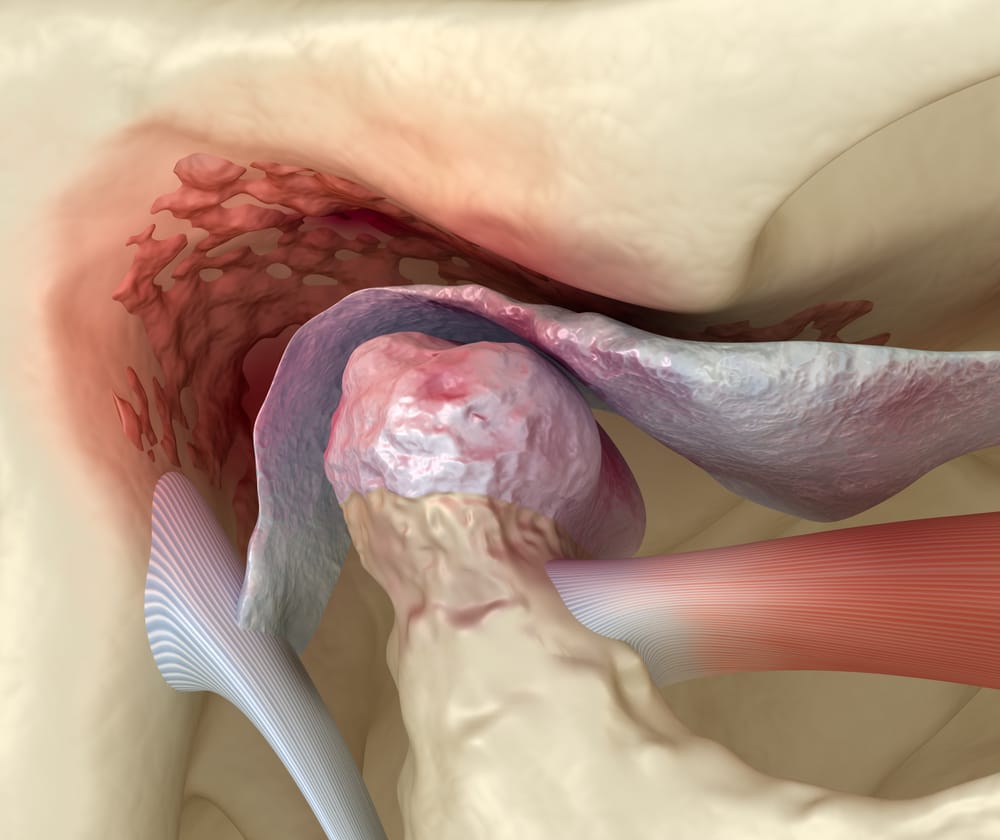 Condylar resorption causes bone loss in the condyles. This can shorten the posterior part of the face.iv Patients seeking help may have observed that their lower jaw has shrunk, leading to a change in their bite. The condition is rare, but has many risk factors:
Condylar resorption causes bone loss in the condyles. This can shorten the posterior part of the face.iv Patients seeking help may have observed that their lower jaw has shrunk, leading to a change in their bite. The condition is rare, but has many risk factors:
Another risk factor is age and hormonal changes. Condylar resorption is nine times more common in women than in men, with a high prevalence for those aged between 10-20.v Pregnancy and other hormonal changes are also associated with the disease. However, it can be spontaneous.iv
Around 60-70% of the UK population will experience some form of TMD in their lifetime.[vi] 2% of people with TMD will also report a limitation with opening their jaw, causing pain and impairing function.iii Condylar resorption is a major factor for the closed lock of the TMJ, making it an essential risk for practitioners to help vulnerable patients with.iii
The progression of degenerative joint disorders leads to changes in the condyle, such as flattening and erosion. In a case study of TMJ arthralgia, 59.6% of cases also had condylar erosion, whilst only 21.2% of asymptomatic patients had it.iii This can lead to notable joint sounds, headaches, pain, and irregular or deviating jaw function.iii
As changes in the condyle alters the TMJ, condyle resorption can cause malocclusion.vii An imperfect bite can disrupt load-bearing capacity, further contributing to TMD and restricting the jaw from opening.viii This can increase the risk of tooth decay and tooth loss.ix
To lower the risk of decay and tooth loss, practitioners should consider recommending at-risks patients for assessment of condylar resorption.
For a diagnosis, a medical professional will take cone beam computed tomography (CBCT) scans of the TMJs to visualise the key features of condylar resorption.iv There are many factors to consider, including the history of the patient, the family history of autoimmune diseases, lifestyle choices, and medications.
Diagnosed patients can be guided through the various ways of managing the disease. This can include anti-inflammatory medications, along with bite splints or night guards to prevent further damage from teeth grinding. For longer-term solutions, orthodontic treatments can correct the bite and orthognathic surgery can align the upper and lower jaw.iv

TMDs can be painful, affecting mood and lowering a patient’s quality of life. For an excellent physical therapy solution, recommend the OraStretch® Press Jaw Rehab System from Total TMJ. The hand-operated device is user-operated; a simple squeeze of the handles stretches the oral cavity to mobilise the TMJ. When following the suggested treatment options, the device improves jaw function, reducing pain and restoring strength. With a transportable solution like this, patients can be empowered to control their health and return to a better quality of life.
For more details about Total TMJ and the products available, please email info@totaltmj.co.uk
i Erwin, J. and Varacallo, M. (2020). Anatomy, Shoulder and Upper Limb, Wrist Joint. [online] PubMed. Available at: https://www.ncbi.nlm.nih.gov/books/NBK534779/.
ii Physiopedia (2009). TMJ Anatomy. [online] Physiopedia. Available at: https://www.physio-pedia.com/TMJ_Anatomy.
iii Emshoff, R., Bertram, F., Schnabl, D., Stigler, R., Steinmaßl, O. and Ansgar Rudisch (2016). Condylar Erosion in Patients With Chronic Temporomandibular Joint Arthralgia: A Cone-Beam Computed Tomography Study. 74(7), pp.1343.e1–1343.e8. doi:https://doi.org/10.1016/j.joms.2016.01.029.
iv What is Condylar Resorption? — condylarresorption.org (2014). condylarresorption.org. [online] condylarresorption.org. Available at: https://www.condylarresorption.org/whatiscondylarresorption.
v Cleveland Clinic. (n.d.). Condylar Resorption: Definition, Treatment & Symptoms. [online] Available at: https://my.clevelandclinic.org/health/diseases/22807-condylar-resorption.
vi Conville, R.M., Moriarty, F. and Atkins, S. (2019). The management of temporomandibular disorders: a headache in general practice. British Journal of General Practice, 69(687), pp.523–524. doi:https://doi.org/10.3399/bjgp19x705977.
vii Min, C.-K., Kim, K.-A., Lee, K.-E., Suh, B.-J. and Jung, W. (2024). A study on volumetric change of mandibular condyles with osteoarthritis using cone-beam computed tomography. Scientific Reports, [online] 14(1). doi:https://doi.org/10.1038/s41598-024-60404-z.
viiiDavid Faustino Ângelo, Maria Cristina Faria-Teixeira, Maffia, F., Sanz, D., Sarkis, M., Marques, R., Mota, B., Ricardo São João and Henrique José Cardoso (2024). Association of Malocclusion with Temporomandibular Disorders: A Cross-Sectional Study. Journal of Clinical Medicine, [online] 13(16), pp.4909–4909. doi:https://doi.org/10.3390/jcm13164909.
ix Gaikwad, S.S., Anjali Gheware, Laxmikant Kamatagi, Sandeep Pasumarthy, Pawar, V. and Madhura Fatangare (2014). Dental Caries and its Relationship to Malocclusion in Permanent Dentition Among 12-15 Year Old School Going Children. Journal of International Oral Health : JIOH, [online] 6(5), p.27. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC4229825/.