
As one of the leading causes of orofacial pain, temporomandibular joint disorder (TMD) is a major disruptor to everyday life.[i] Whether limiting the choice of foods or causing consistent pain, the impact of TMD is widespread.
Sleep bruxism has a correlation with TMD that demands closer attention. This is a contentious link that can often provide divisive results.
TMD easily progresses from acute to chronic pain. The temporomandibular joint (TMJ) is used throughout the day for talking and eating.
Bruxism is characterised as repetitive jaw-muscle activity, such as the bracing or thrusting of the mandible and grinding. This is self-reported among 12% of the population.[i]
Research on the association between the two conditions is divisive. One study found that the methodologies used heavily influenced each paper’s findings. For example, those based on a self-reported or questionnaire-based approach to bruxism found an association with TMD.[ii] This highlights the need for more specific categorisations of both conditions.
For sleep bruxism, the Internal Classification of Sleep Disorders has established criteria. It notes:
Almost 40% of patients with TMD pain are told by their dentist that they have sleep bruxism. These patients are expected to report a higher pain intensity.
Peak incidence of sleep bruxism is among adults aged 20-40.[i] This is the age for raising a family, finding jobs, owning property and juggling busy social lives. It is unsurprising then that sleep bruxism is linked to elevated levels of stress, anxiety and depression – there’s a lot to manage as an adult.
Those with higher levels of stress are likelier to grind their teeth, but not every sleep bruxer will fall into the cycle of disrupted sleep, impacted mood and TMJ pain. Some studies state that bruxism itself is a mechanism for stress relief, and does not cause it.[i]
For dental professionals, identifying patients who have a higher risk of developing TMD or are showing signs of sleep bruxism is vital. The leading predictors for both conditions are:
With these in mind, dental professionals can guide patients towards suitable management strategies.
Whilst the research around sleep bruxism demonstrates that it may not be a direct cause of TMD, the correlation between the two makes them excellent indicators for the other.
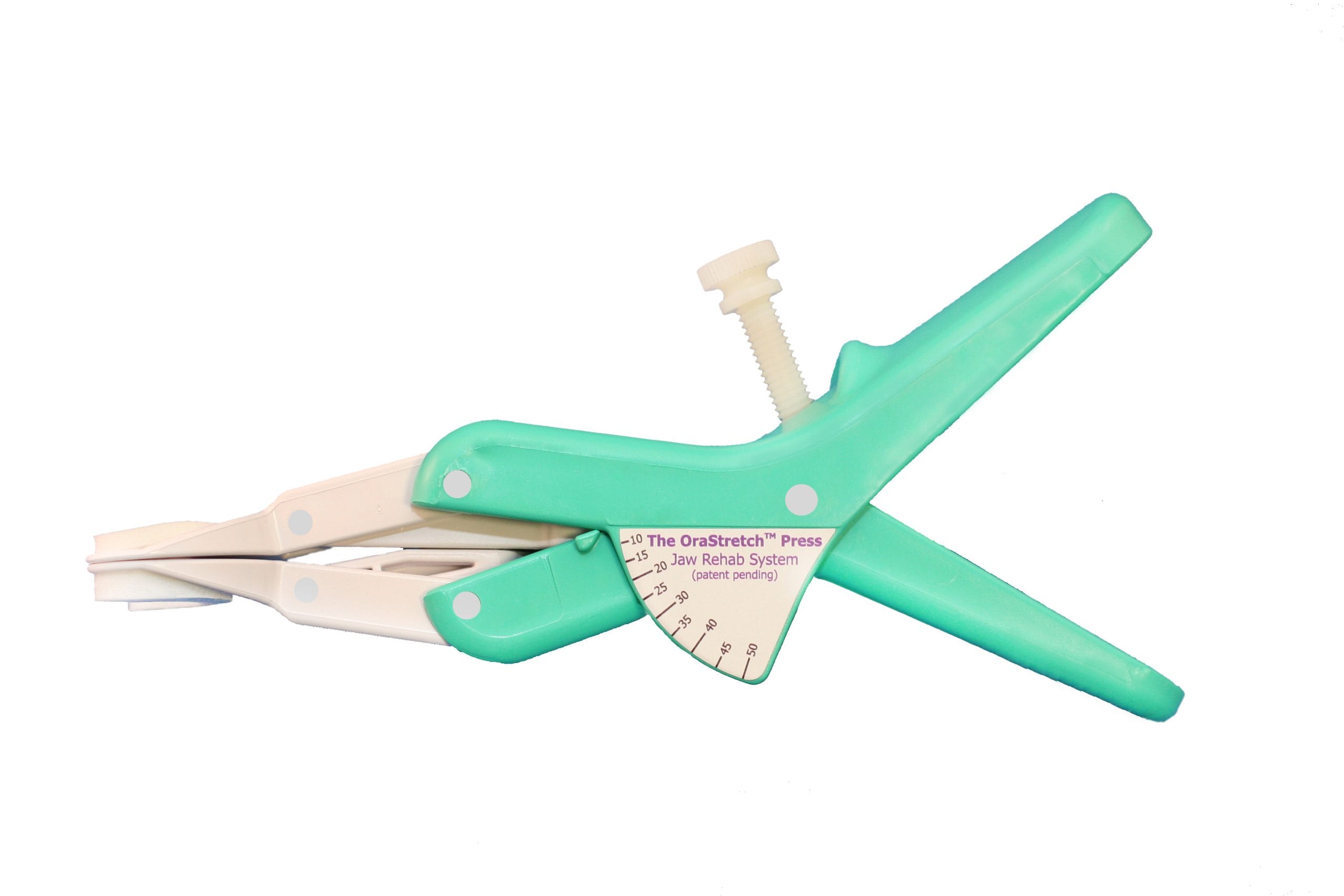
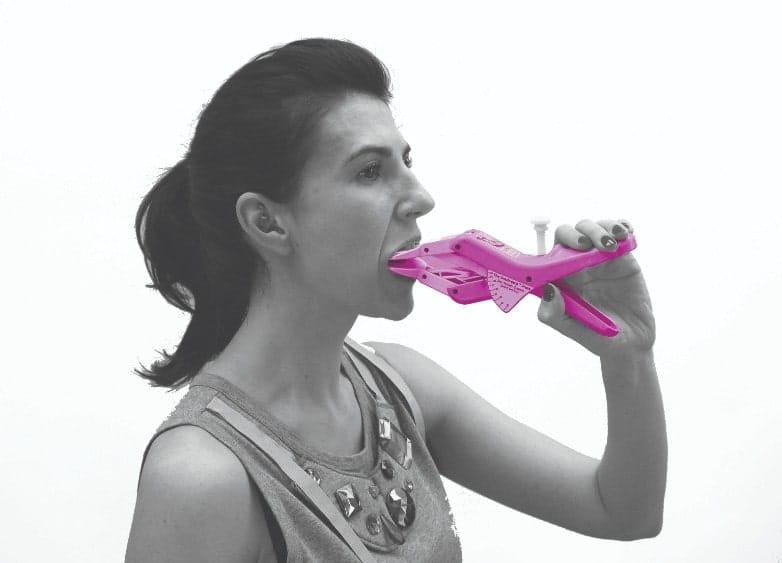
To help patients alleviate the symptoms of TMD and restore strength and function to the jaw, recommend the OraStretchâ Press Rehab System from Total TMJ. A reliable device for at-home rehabilitation, it stretches the orofacial tissues to promote mobility. Diligent use can lead to an improved quality of life, one where jaw pain is no longer a major disruptor to everyday activities – especially sleep.
Whilst easy to look at the overlapping risk factors between TMD and sleep bruxism, the actual cause and effect between the two continues to be controversial. Dental practitioners can help by assessing at-risk patients and highlighting the best ways to limit sleep bruxism and manage TMD for a better night’s sleep and an improved quality of life.
[i] Lee, Y.-H., Chon, S., Q-Schick Auh, Verhoeff, M.C. and Lobbezoo, F. (2025). Clinical, psychological, and hematological factors predicting sleep bruxism in patients with temporomandibular disorders. Scientific Reports, [online] 15(1). doi:https://doi.org/10.1038/s41598-025-03339-3.
[ii] Manfredini, D. and Lobbezoo, F. (2021). Sleep bruxism and temporomandibular disorders: A scoping review of the literature. Journal of Dentistry, 111, p.103711. doi:https://doi.org/10.1016/j.jdent.2021.103711.
[iii] Ohlmann, B., Waldecker, M., Leckel, M., Bömicke, W., Behnisch, R., Rammelsberg, P. and Schmitter, M. (2020). Correlations between Sleep Bruxism and Temporomandibular Disorders. Journal of Clinical Medicine, 9(2), p.611. doi:https://doi.org/10.3390/jcm9020611.