The jaw has many important functions biologically. The temporomandibular joint (TMJ) connects the jawbone to the skull. It’s what allows you to talk, eat, and yawn. Patients shouldn’t ignore jaw pain, clicking, stiffness, or chronic headaches. These symptoms could be something far bigger than they seem: Temporomandibular disorder (TMD).
Whilst arthritis or physical trauma can cause TMD, every day, normal habits can too. For general dental practitioners, early identification of related symptoms is important. From this, symptoms can be managed and treatment can be planned.

TMD is a common but painful condition, and often under-diagnosed. Symptoms include jaw pain, struggles opening the mouth, and even migraines. Estimates suggest that between 5% and 12% of the population experience TMD symptoms.[i]
Inflammation, unusual oral habits, physical trauma, muscular tension, and psychological stress causes TMD. The issue can go undiagnosed or misdiagnosed as sinus pain or general stress.[ii] It’s important to recognise inhibiting factors that can cause or make pain worse over time.
Several seemingly harmless habits can increase the risk of developing or worsening TMD. Though innocuous, patients should avoid and minimise these habits. It is widely understood that bruxism is one of the major risk factors for TMD.[i] This teeth-grinding can happen both when awake or asleep. Stress and poor sleeping habits can make it worse.
Poor posture is another habit that makes TMD worse.[ii] A forward-head position disrupts the alignment between your jaw, neck, and shoulder muscles.[iii] Phone or computer use can cause this imbalance and can worsen symptoms over time.
Other parafunctional oral habits like biting nails, chewing on pencils, and resting the chin on the hand can seem harmless. Yet, the repeated stress on the jaw muscles and surrounding joints can cause inflammation and muscle fatigue.[iv] Stress and anxiety elevate muscle tension in the head, neck, and jaw, subconsciously increasing clenching, or lip biting. Due to how subliminal these habits are, stress and anxiety are one of TMD’s most harmful factors.
Another major area for concern is dry mouth. A survey on people born with a cleft reported that 54% were regular snorers.[iv] A further 61% of the participants stated that they regularly wake up with a dry mouth. Mouth breathing, especially for long periods at night, dries out the mouth. As saliva helps protect the teeth from decay, a lack of it increases the risk of oral disease.
Impacted diet is also a cause for concern. 27% of patients born with a cleft avoid certain foods.[iv] This is often hard, small or spicy options. Limited food choice can lead to an unhealthy diet, increasing the risk of health complications and oral disease.[i] To prevent this, a consistent oral hygiene routine must be encouraged in cleft lip and palate patients from a young age.
Those experiencing constant jaw pain, constrained opening, frequent clicking, or pressure will require a professional evaluation. Early assessments by a dentist can prevent escalation of the problem to chronic status.

Before needing to seek professional help, adaptations can have a significant impact on a patient’s experience with TMD. Primarily, minimising parafunctional habits: nail or pencil biting and resting the jaw upon the hand. Furthermore, stress management, through mindfulness or breathing techniques, can also assist.
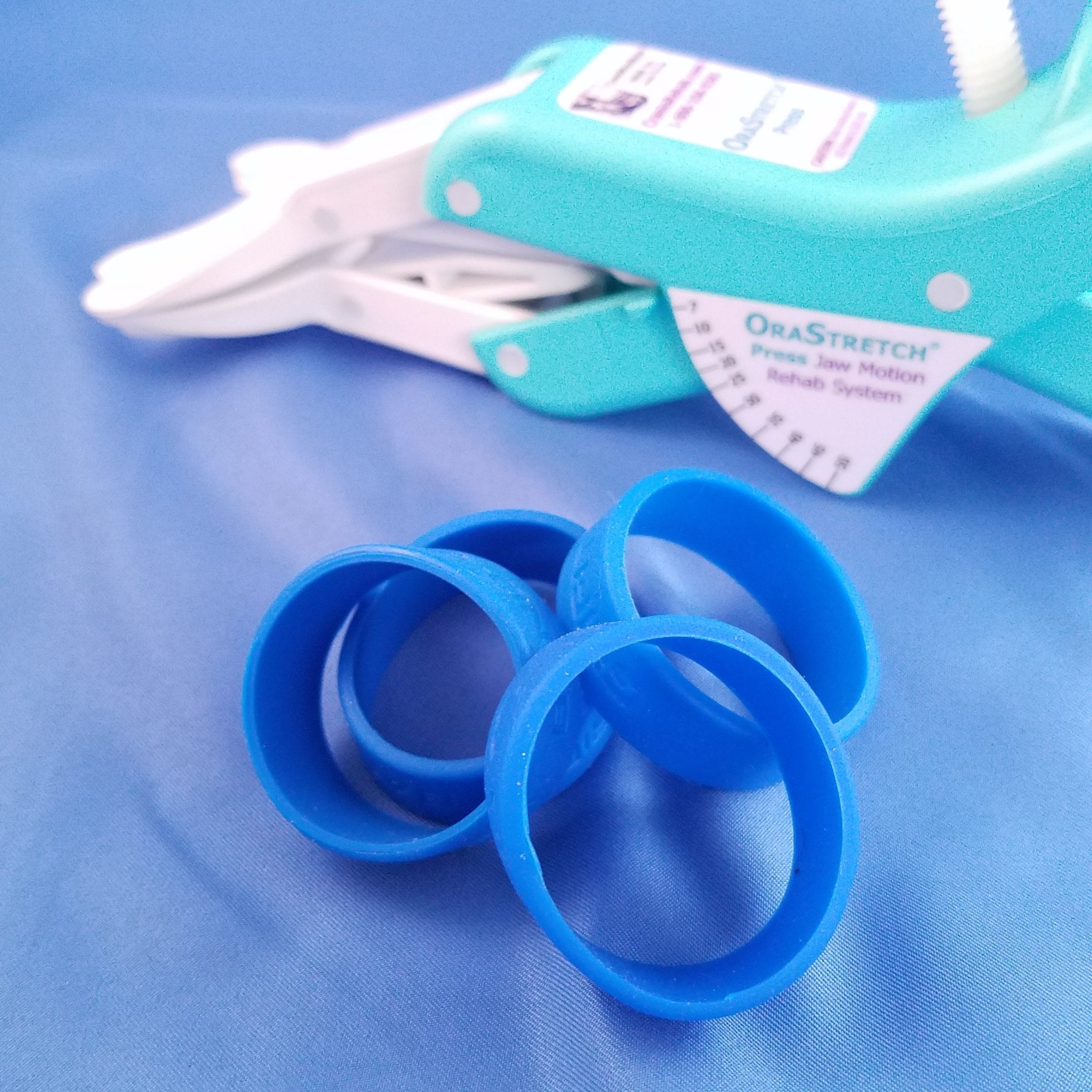
For those seeking guided physical support, solutions like the OraStretch® Press Rehab System from Total TMJ are perfect. This tool helps to encourage jaw mobility and recovery without forceful movement. The device offers innovation from home, giving patients reclaimed power over their recovery. Its passive stretching abilities mobilise the TMJ to regain muscle strength and enhance jaw function. Within a week, users can expect to see rehabilitation results, and gain 1-2mm of jaw range of motion back.
While TMD can be painful and disruptive, it’s often manageable by changing everyday habits. From improving posture to breaking unconscious behaviours, each adjustment can help hugely. Raising awareness of these triggers, with proactivity, offers the best chance in preventing escalation of symptoms.
[i] Cleft. (n.d.). Cleft lip and palate. [online] Available at: https://www.cleft.org.uk/pages/faqs/category/faqs.
[ii] Wu, Q., Li, Z., Zhang, Y., Peng, X. and Zhou, X. (2022). Dental caries and periodontitis risk factors in cleft lip and palate patients. Frontiers in Pediatrics, [online] 10, p.1092809. doi:https://doi.org/10.3389/fped.2022.1092809.
[iii] NHS (2019). Overview – Cleft lip and palate. [online] NHS. Available at: https://www.nhs.uk/conditions/cleft-lip-and-palate/.
[iv] World Health Organization (2023). Unhealthy diet. [online] World Health Organization – Regional Office for the Eastern Mediterranean. Available at: https://www.emro.who.int/noncommunicable-diseases/causes/unhealthy-diets.html.
[i] Matheson, E. M., Fermo, J. D., & Blackwelder, R. S. (2023). Temporomandibular Disorders: Rapid Evidence Review. American family physician, 107(1), 52–58.
[ii] Kanehira, H., Agariguchi, A., Kato, H., Yoshimine, S., & Inoue, H. (2008). Association between stress and temporomandibular disorder. Japanese Journal of Prosthodontics, 52(3), 375–380. https://doi.org/10.2186/jjps.52.375
[iii] Poveda Roda, R., Bagan, J. V., Díaz Fernández, J. M., Hernández Bazán, S., & Jiménez Soriano, Y. (2007). Review of temporomandibular joint pathology. Part I: classification, epidemiology, and risk factors. Medicina oral, patologia oral y cirugia bucal, 12(4), E292–E298.
[iv] Minervini, G., Franco, R., Marrapodi, M. M., Crimi, S., Badnjević, A., Cervino, G., Bianchi, A., & Cicciù, M. (2023). Correlation between Temporomandibular Disorders (TMD) and Posture Evaluated trough the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD): A Systematic Review with Meta-Analysis. Journal of clinical medicine, 12(7), 2652. https://doi.org/10.3390/jcm12072652
[v] Xiao, C.-Q., Wan, Y.-D., Li, Y.-Q., Yan, Z.-B., Cheng, Q.-Y., Fan, P.-D., Huang, Y., Wang, X.-Y. and Xiong, X. (2023). Do Temporomandibular Disorder Patients with Joint Pain Exhibit Forward Head Posture? A Cephalometric Study. Pain Research and Management, 2023, pp.1–11. doi:https://doi.org/10.1155/2023/7363412.
[vi] Šimunović, L., Lapter Varga, M., Negovetić Vranić, D., Čuković-Bagić, I., Bergman, L., & Meštrović, S. (2024). The Role of Malocclusion and Oral Parafunctions in Predicting Signs and Symptoms of Temporomandibular Disorders—A Cross-Sectional Study. Dentistry Journal, 12(7), 213. https://doi.org/10.3390/dj12070213